
Every Step You Take
Neuropathy & Foot Clinic of Los Angeles
Peripheral Neuropathy Treated by Podiatrists in Los Angeles: Symptoms & Solutions
Are you dealing with muscle weakness or tingling sensations in your feet? Podiatrists at the Neuropathy & Foot Clinic of Los Angeles specialize in diagnosing and treating peripheral neuropathy, particularly when it impacts the feet and lower extremities.
Peripheral neuropathy damages nerves and causes symptoms like muscle weakness, tingling, and pain, often affecting the hands and feet first.
Podiatrists play a crucial role in diagnosing and managing this painful condition through thorough examinations, custom orthotics, physical therapy, and patient education.
Managing symptoms involves personalized treatments like pain relief creams, exercises to improve muscle strength, and innovative therapies such as nerve stimulators and laser treatments.
Understanding Peripheral Neuropathy
It involves damage to the peripheral nervous system, which is responsible for transmitting information between the central nervous system (the brain and spinal cord) and the rest of the body. When these peripheral nerves are damaged, the communication between the brain and other body parts is disrupted, leading to muscle weakness, tingling, and pain in the extremities, particularly the hands and feet. This condition can arise from various causes, including traumatic injuries, infections, metabolic disorders, inherited conditions, and exposure to toxins. Additionally, it can be a result of autoimmune diseases such as Sjogren’s syndrome, lupus, and rheumatoid arthritis.
The symptoms of peripheral neuropathy are diverse and can manifest as numbness, prickling, or tingling in the feet or hands, which may eventually spread to the legs and arms. Many individuals describe their pain as stabbing, burning, or tingling. Beyond pain, it can affect other bodily functions, such as digestion and urination. Effectively diagnosing and managing the condition requires a deep understanding of these symptoms and their underlying causes.

Types of Peripheral Neuropathy
It can be broadly classified into inherited and acquired types. Inherited peripheral neuropathies, such as Charcot-Marie-Tooth disease, are genetic and present from birth. On the other hand, acquired peripheral neuropathies develop due to external factors like injuries, infections, or underlying health conditions, such as chronic inflammatory demyelinating polyneuropathy.
Additionally, it can affect one nerve (mononeuropathy), two or more nerves in different areas (multiple mononeuropathy), or many nerves (polyneuropathy). For instance, diabetic neuropathy typically affects multiple nerves and can lead to significant discomfort and disability.
Peripheral neuropathy can also be categorized based on the type of nerve fibers affected—sensory, motor, or autonomic.
Sensory neuropathy affects the sensory nerves responsible for touch, pain, temperature, and position sense, leading to symptoms like numbness and tingling.
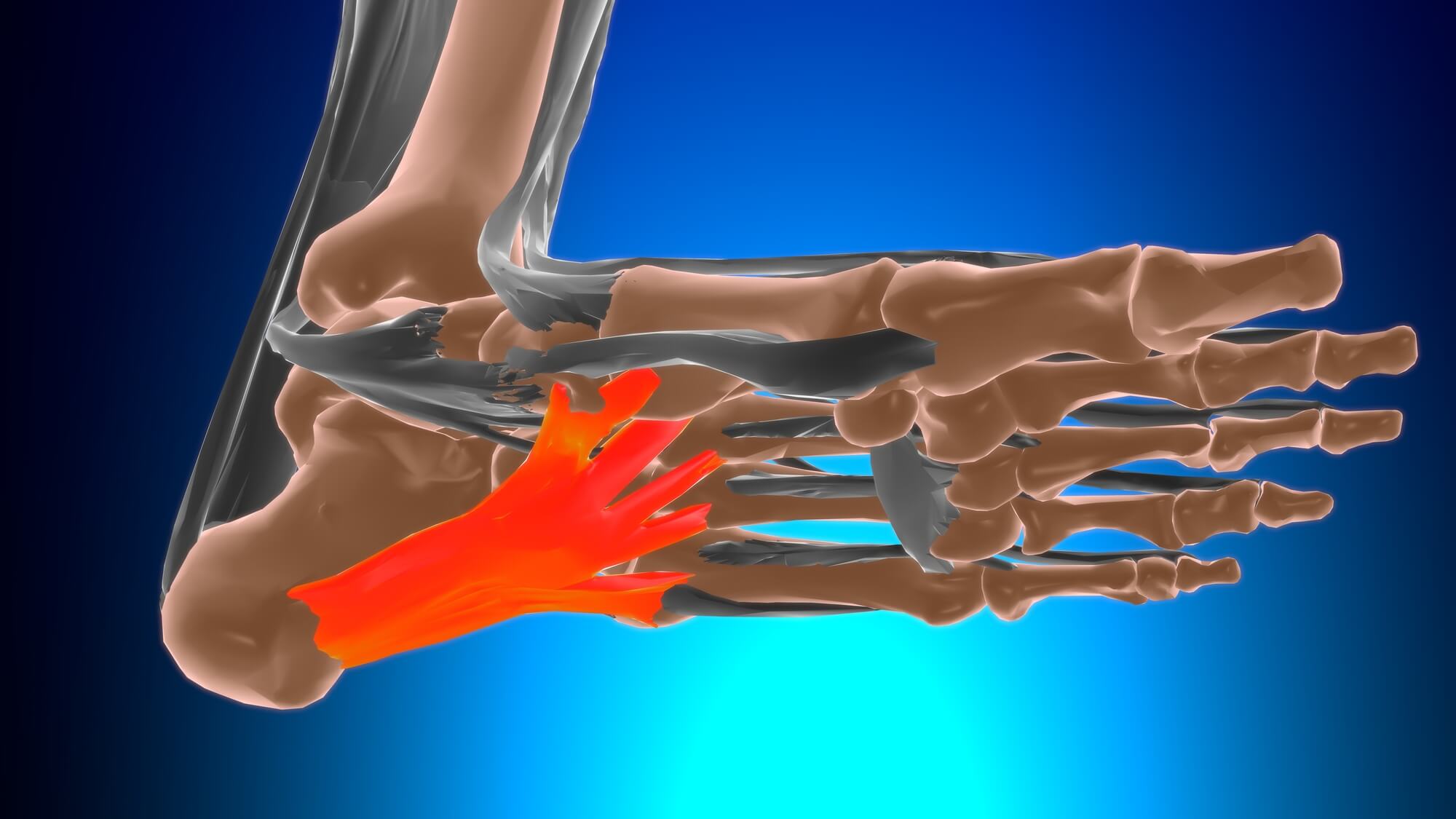
Motor neuropathy impacts the motor nerves that control muscle movements, resulting in muscle weakness and atrophy.
Autonomic neuropathy affects the autonomic nerves that regulate involuntary functions such as heart rate, blood pressure, and digestion.
A clear comprehension of these types is beneficial in adapting treatment approaches to the patient’s specific needs.
The Role of Podiatrists in Los Angeles in Treating Peripheral Neuropathy
Podiatrists are medical professionals who specialize in foot and ankle health, making them key players in managing this condition. Given that peripheral neuropathy often manifests in the feet, podiatrists are uniquely positioned to diagnose and treat this condition with tailored care plans. Their expertise extends beyond simple foot care; they offer comprehensive assessments, monitor the progression of the condition, and provide crucial education on maintaining foot health. This specialized care is particularly vital for diabetic patients, as it aids in preventing complications and promoting overall well-being.
One of the critical roles of podiatrists is to teach patients how to care for their feet at home. This includes advising on proper footwear, demonstrating foot hygiene practices, and recommending exercises to maintain foot strength and flexibility. Podiatrists educate patients to empower them, enabling proactive steps in managing their condition and potentially preventing further deterioration.
A multi-faceted process begins with a thorough physical examination and a review of the patient’s health history. Podiatrists check for reflexes, sensation, and muscle strength in the feet and legs.
They look for signs like diminished reflexes and reduced sensitivity to touch, which are indicative of nerve damage. Patients may also be asked about their symptoms, including the onset, duration, and intensity of pain or numbness.
In addition to physical exams, podiatrists often use blood tests to identify underlying causes of peripheral neuropathy, such as high blood sugar levels in diabetic patients. These tests help in pinpointing whether the neuropathy is related to diabetes, vitamin deficiencies, or other metabolic conditions. Using these diagnostic tools in combination, podiatrists can gain a comprehensive understanding of the patient’s condition and accordingly customize a treatment plan.
Once a diagnosis is made, podiatrists employ a variety of treatments to manage the symptoms. Custom orthotics are commonly used to relieve pressure on specific areas of the foot and help maintain proper foot positioning. These orthotic devices can significantly reduce pain and prevent further injury by providing adequate support during walking and other activities.
Physical therapy is another cornerstone treatment, aimed at improving balance, strength, and mobility. Podiatrists may also prescribe oral medications to manage neuropathic symptoms, including pain. In some cases, transcutaneous electrical nerve stimulation (TENS) is used. This technique involves applying electrical currents to the skin to block pain signals and provide relief.
Utilizing these diverse peripheral neuropathy treatments enables podiatrists to address the complex nature of this disease and enhance their patients’ quality of life.
It’s especially vital to manage the symptoms of when the underlying cause cannot be treated. Podiatrists play a vital role in this management through specialized foot care techniques. Proper foot care is essential, particularly for individuals with diabetes, to minimize pain and prevent complications such as sores and infections. Techniques like wearing soft, loose-fitting cotton socks and padded shoes can make a significant difference in comfort and mobility.
Massaging the feet can also improve circulation and provide temporary relief from pain. These simple yet effective strategies, combined with professional podiatric care, can help manage the symptoms and enhance the patient’s quality of life.
The following subsections will delve into specific strategies for pain management, addressing muscle weakness, and controlling excessive sweating.
Pain Management Techniques
Pain management is a critical component of treating peripheral neuropathy. Podiatrists often recommend topical treatments such as capsaicin cream and lidocaine patches to alleviate discomfort. Capsaicin cream works by depleting a neurotransmitter called substance P, which is involved in transmitting pain signals. Lidocaine patches provide localized pain relief by numbing the affected area. These treatments can be particularly effective in managing mild to moderate neuropathic pain.
For more severe pain, podiatrists may prescribe neuropathic agents, including certain medications initially developed for other conditions, such as anti-seizure drugs. These medications help to modulate the nervous system and reduce chronic pain. Podiatrists can adapt pain management strategies to the individual needs of their patients by using a combination of topical and oral treatments.
Addressing Muscle Weakness
Muscle weakness is a common issue in these patients. Podiatrists address this by prescribing specific exercises designed to strengthen the muscles weakened by nerve damage. These exercises focus on rebuilding muscle tissue and improving overall foot and leg function. Regular practice of these exercises can lead to significant improvements in mobility and strength.
In addition to exercises, podiatrists may recommend the following supportive devices to stabilize weakened muscles:
- Braces
- Orthotics
- Shoe inserts
- Ankle supports
These devices help maintain proper alignment and reduce the risk of falls and other injuries. Combining exercises with supportive devices enables patients to gain superior control over their movements and improve their daily activities.
Solutions for Excessive Sweating
Excessive sweating, or hyperhidrosis, is another symptom that can significantly affect the comfort and quality of life for those with peripheral neuropathy. Podiatrists often use botulinum toxin (Botox) injections to manage this condition effectively. Botox works by blocking the nerves responsible for activating sweat glands, thereby reducing excessive sweating.
In addition to Botox, podiatrists may explore other treatments for hyperhidrosis to ensure patient comfort. These might include antiperspirants, medications, or even surgical options in severe cases. It’s essential to manage excessive sweating to prevent associated complications and enhance the overall well-being of neuropathy patients.

Preventative Measures and Lifestyle Changes
Peripheral neuropathy prevention necessitates a proactive approach towards managing underlying conditions and maintaining a healthy lifestyle. Significant nerve health support and neuropathy onset or progression prevention can be achieved through:
- Quitting smoking
- Avoiding toxins
- Engaging in regular exercise
- Maintaining a balanced diet
Particularly, the management of underlying medical conditions, like diabetes, is vital.
A diet rich in nutrients, such as fish, nuts, whole grains, and fresh produce, can help maintain a healthy weight and reduce the risk of neuropathy. Regular exercise not only improves muscle strength and reduces pain but also helps control blood sugar levels, which is essential in managing and preventing peripheral neuropathy. Avoiding excess alcohol and maintaining good foot hygiene are additional steps that can prevent complications and improve quality of life.
Blood Sugar Control
For individuals with diabetes, blood sugar control is paramount in preventing nerve damage and reducing the symptoms of peripheral neuropathy. High blood sugar levels can damage the small blood vessels that supply nerves, leading to diabetic neuropathy. Keeping blood glucose levels within a healthy range can encourage nerve regeneration and reduce neuropathy symptoms.
Careful management of diabetes through regular monitoring, medication, and lifestyle changes can prevent or reduce further nerve damage. Maintaining healthy blood sugar levels is not only critical for preventing diabetic neuropathy but also for overall health and well-being. Patients can make significant strides towards preventing neuropathy and its associated complications by giving priority to blood sugar control.
Healthy Diet and Exercise
A healthy diet and regular exercise are cornerstones of preventing and managing peripheral neuropathy. Nutritional supplements like B vitamins, vitamin E, and omega-3 fatty acids support nerve health and reduce inflammation. A balanced diet that includes these nutrients can correct deficiencies and improve gastrointestinal symptoms caused by neuropathy.
Regular physical activity enhances nerve health by improving blood flow and reducing inflammation. Combined with a balanced diet, exercise helps maintain healthy blood sugar levels, which is crucial for preventing neuropathy. Adopting a healthy lifestyle enables individuals to significantly lower their risk of developing it and more effectively manage existing symptoms.
When to See a Podiatrist
Consulting a podiatrist becomes essential if you experience:
- Persistent pain, numbness, or tingling in your feet
- Unusual sensitivity to touch
- Coordination problems
- Persistent or worsening numbness
Early detection and treatment can prevent further complications and improve quality of life. It is important not to ignore persistent or worsening numbness, as it can indicate progressive nerve damage.
Frequent or severe foot pain that interferes with daily activities is another red flag. Seeing a podiatrist early allows for a comprehensive evaluation and an appropriate treatment plan to effectively manage your symptoms. The following subsections will discuss the early signs to watch for and how to prepare for your appointment.
Early Signs to Watch For
Early signs of peripheral neuropathy include:
- Unusual tingling, weakness, or pain in the hands or feet
- A gradual onset of numbness, prickling, or tingling in the feet
These sensory symptoms may eventually spread to the legs and arms, making early detection crucial.
Burning sensations, cramps, and muscle spasms are also significant indicators of neuropathy-related muscle weakness. If you notice any of these symptoms, it’s important to seek medical advice promptly. Early intervention can prevent the progression of peripheral neuropathy and improve outcomes.
How to Prepare for Your Appointment
Preparing for your appointment with a podiatrist can ensure a productive and comprehensive evaluation. Here are some things to do before your appointment:
- Bring a list of all medications and supplements you’re currently taking.
- Bring a record of your medical history.
- Be prepared to discuss any underlying conditions or treatments that could be contributing to your symptoms.
This information will help the podiatrist understand your situation better and provide appropriate treatment.
Additionally, when visiting your podiatrist, it is important to:
List all your symptoms, even those that may not seem related, to provide a complete picture of your health.
Prepare specific questions about your symptoms, potential causes, and treatment options.
Come well-prepared to maximize your appointment and collaborate with your podiatrist to formulate an effective treatment plan.
Advanced Treatment Options
For those with severe peripheral neuropathy, advanced treatment options are available to address the underlying causes and alleviate symptoms. These treatments go beyond standard care and can include innovative therapies and surgical interventions. Podiatrists may recommend nerve decompression surgery or regenerative medicine approaches for significant symptom relief.
Innovative therapies, such as peripheral nerve stimulators and laser treatments, are designed to stimulate tissue repair, increase blood flow, and reduce inflammation. These cutting-edge treatments offer new hope for patients with chronic pain and severe symptoms.

Surgical Interventions
Surgical interventions are considered for severe cases of peripheral neuropathy where conservative treatments have failed. Procedures that can alleviate symptoms and improve nerve function include:
- Carpal tunnel release
- Internal and external neurolysis
- Nerve grafting
- Nerve decompression surgery, which relieves pressure on nerves
These surgical options can significantly reduce pain and improve mobility.
These surgical options involve making small incisions to relieve pressure and can provide immediate relief from pain and numbness. Addressing the structural causes of nerve compression through these surgeries can yield long-term benefits for patients with severe neuropathy.
Innovative Therapies
Innovative therapies aim to enhance nerve function and alleviate symptoms through advanced techniques. Peripheral nerve stimulators, implanted through minimally invasive procedures, are effective for managing chronic nerve pain. These devices provide electrical stimulation to the nerves, helping to reduce pain and improve nerve function.
Laser treatment is another innovative therapy that stimulates tissue repair at the cellular level, increasing blood flow and reducing inflammation. Vibration therapy, which uses vibrating devices to promote circulation and nerve function, can also help alleviate symptoms such as pain and numbness. These advanced therapies offer new avenues for relief and improved quality of life for patients with peripheral neuropathy.
Summary
Peripheral neuropathy is a complex and multifaceted condition that requires a comprehensive approach to diagnosis and treatment. Podiatrists play a crucial role in managing this condition through specialized care, tailored treatment plans, and advanced therapies. By understanding the symptoms, types, and preventative measures, patients can take proactive steps towards better foot health and overall well-being. Whether through lifestyle changes, pain management techniques, or advanced treatment options, there are numerous ways to alleviate the symptoms and improve quality of life. Take charge of your health today and consult with a podiatrist to explore the best options for managing your condition.
Frequently Asked Questions
Common symptoms include numbness, prickling, or tingling in the feet or hands, which may spread to the legs and arms, along with pain described as stabbing, burning, or tingling. If you experience these, it’s important to consult a healthcare professional.
They look for signs like diminished reflexes and reduced sensitivity to touch, which are indicative of nerve damage. Patients may also be asked about their symptoms, including the onset, duration, and intensity of pain or numbness.
In addition to physical exams, podiatrists often use blood tests to identify underlying causes of peripheral neuropathy, such as high blood sugar levels in diabetic patients. These tests help in pinpointing whether the neuropathy is related to diabetes, vitamin deficiencies, or other metabolic conditions. Using these diagnostic tools in combination, podiatrists can gain a comprehensive understanding of the patient’s condition and accordingly customize a treatment plan.
Podiatrists diagnose peripheral neuropathy by conducting physical exams, reviewing medical history, and performing blood tests to identify underlying causes. These tests help them determine the extent and potential causes of the condition.
Podiatrists offer treatments such as custom orthotics, physical therapy, oral medications, and advanced options like TENS, depending on the individual’s condition and needs. These treatments can help manage symptoms and improve quality of life.
Making lifestyle changes such as quitting smoking, exercising regularly, maintaining a balanced diet, and managing underlying conditions like diabetes can help prevent peripheral neuropathy. These changes are crucial in maintaining nerve health.
You should see a podiatrist if you have persistent pain, numbness, or tingling in your feet that interferes with your daily activities. It’s important to address these symptoms promptly.
Podiatrists in Los Angeles CA: Essential Services and Treatments Explained
Podiatrists are healthcare professionals specializing in the diagnosis and treatment of foot and ankle issues. They offer various services, including diagnosing conditions, providing non-surgical and surgical treatments, and offering preventive care and education. By understanding how they can assist with your foot health, you can make informed decisions about your care.
Now, you might be thinking, “Why would I need to see a foot doctor?” Well, you’d be surprised at how many different services podiatrists offer. From treating everyday foot pain to performing complex surgeries, these docs do it all. So, let’s take a stroll through the world of podiatry and explore the main services these foot specialists provide. Trust me, by the end of this, you’ll have a new appreciation for these masters of the lower extremities!
Diagnosis and treatment of foot disorders:
So, you know how your feet can sometimes give you trouble? Well, that’s where podiatrists come in. They’re like foot detectives, figuring out what’s causing your pain or discomfort. Whether it’s those pesky bunions that make your shoes feel tight, or that nagging heel pain that just won’t quit, podiatrists have got your back (or should I say, your feet?). They’ll examine your feet, maybe do some tests, and then come up with a plan to get you back on your feet comfortably.


Diabetic foot care:
For folks with diabetes, taking care of their feet is super important. Diabetes can cause all sorts of foot problems that might not seem like a big deal at first but can become serious if left unchecked. Podiatrists are like the guardians of diabetic feet. They keep an eye out for things like ulcers or nerve damage, help manage any issues that pop up, and teach patients how to take good care of their feet at home. It’s all about preventing small problems from becoming big ones.
Sports medicine:
If you’re into sports or fitness, you know how important your feet are, right? Podiatrists who specialize in sports medicine are like the pit crew for your feet. They help athletes deal with injuries like sprains or stress fractures, and they can give advice on the best shoes for your sport. They’re all about keeping you in the game and helping you perform your best, whether you’re a weekend warrior or a pro athlete.


Toenail Care:
Toenail troubles can be a real pain, right? Whether it’s an ingrown nail that’s making every step uncomfortable, or a fungal infection that’s making you think twice about wearing sandals, podiatrists have seen it all. They can treat these issues quickly and effectively, often right there in the office. Plus, they can give you tips on how to keep your nails healthy and prevent future problems. It’s like a spa day for your feet, but with medical expertise!
Wound care:
For some people, especially those with diabetes or circulation issues, even a small cut on the foot can be a big deal. Podiatrists are experts at managing and treating these wounds. They know all the latest techniques to help wounds heal faster and prevent infections. They’ll work with you to create a treatment plan, which might include special dressings, medications, or even high-tech treatments like hyperbaric oxygen therapy. It’s all about healing those wounds and keeping your feet healthy and strong.


Heel pain treatment:
Let’s talk about heel pain for a second. You know that sharp ache you sometimes feel when you take your first steps in the morning or after sitting for a while? That’s often plantar fasciitis, and it’s just one of the many causes of heel pain that podiatrists deal with regularly. They’re like heel pain detectives, figuring out if it’s coming from a bone spur, a stress fracture, or something else entirely. And once they crack the case, they’ve got a whole toolkit of treatments to help. It might be special stretches, custom orthotics, or even cutting-edge therapies like shockwave treatment. The goal? To have you walking on sunshine again, not on eggshells because of your heels. So if your heels are giving you grief, a podiatrist can be your new best friend.
Bunion treatment and minimally invasive procedures:
Now, let’s chat about bunions – those pesky bumps that can form on the side of your big toe. If you’ve got one, you know they can be a real pain, both literally and when it comes to finding comfortable shoes. Podiatrists are like bunion busters, offering a range of treatments from conservative options to surgical solutions. And here’s some exciting news: minimally invasive bunion surgery is becoming more common. It’s like the laparoscopic surgery of the foot world. Instead of one big incision, the podiatrist makes tiny ones and uses special instruments to correct the bunion. This often means less pain, faster recovery, and smaller scars. So if you’ve been putting off dealing with your bunion because you’re worried about a long, painful recovery, it might be time to chat with a podiatrist about these newer, less invasive options. Who knows? You might be back in your favorite shoes sooner than you think!


Foot and ankle fracture treatment:
Ouch! Fractures in the foot or ankle can really put a damper on your day-to-day life. Whether it’s from a sports injury, a misstep off a curb, or just bad luck, these breaks need expert care. That’s where podiatrists come in – they’re like the puzzle masters of the foot world. They can diagnose and treat all sorts of fractures, from the tiny bones in your toes to the larger bones in your ankle. Depending on the break, treatment might involve anything from a simple boot or cast to surgery for more complex fractures. And it’s not just about healing the bone – podiatrists also focus on preventing long-term issues like arthritis or chronic pain. They’ll work with you on a rehabilitation plan to get you back on your feet (literally) and moving comfortably again. So if you’ve had a mishap and suspect a fracture, don’t hobble around hoping it’ll get better on its own. A podiatrist can help ensure your bones heal properly, potentially saving you from bigger problems down the road.
Orthotics:
Ever wished your shoes could be more, well, you-shaped? That’s kind of what orthotics are all about. Podiatrists can create these custom inserts for your shoes that are like a perfect mold of your feet. They’re not just for comfort (though that’s a nice bonus). These inserts can help correct the way you walk, distribute your weight more evenly, and even alleviate pain in your feet, knees, or back. It’s like having a secret weapon in your shoes!

Summary:
So there you have it – a whirlwind tour of the world of podiatry! As you can see, podiatrists are way more than just “foot doctors.” They’re problem solvers, pain relievers, and sometimes even lifesavers when it comes to conditions like diabetic foot complications. From crafting custom orthotics to performing intricate surgeries, these specialists have a wide range of skills to keep our feet healthy and happy.
Remember, our feet are the foundation of our body, and taking care of them is crucial for our overall health and mobility. Whether you’re dealing with a nagging pain, a sports injury, or just want to make sure your feet are in good shape, a podiatrist can help. So next time your feet are giving you trouble, don’t just walk it off – consider giving a podiatrist a visit. Your feet will thank you!
Frequently Asked Questions
If you are experiencing persistent foot pain, swelling, infections, stress fractures, or chronic heel pain, it’s time to see a podiatrist for professional help. Don’t ignore these signs.
Podiatrists diagnose foot and ankle issues through physical exams, imaging tests like X-rays and MRIs, and by assessing recent activities. This helps them develop an accurate diagnosis and appropriate treatment plan.
Podiatrists offer non-surgical treatments such as orthotic shoe inserts, physical therapy, and the management of conditions like ingrown toenails using topical treatments and proper footwear. These measures can help address foot issues without the need for surgery.
Make sure to maintain good foot hygiene, wear properly fitting shoes, and conduct regular self-examinations to keep your feet healthy and prevent issues. This will help you avoid foot problems and stay comfortable on your feet.
Podiatrists manage diabetic foot complications by performing routine foot examinations, nerve sensitivity checks, circulation assessments, and offering advanced treatments for ulcers and peripheral neuropathy. This helps to prevent and address complications associated with diabetes.
